Date: January 11, 2026
By: Jude Chartier / [AI Nurse Hub]
I. Introduction
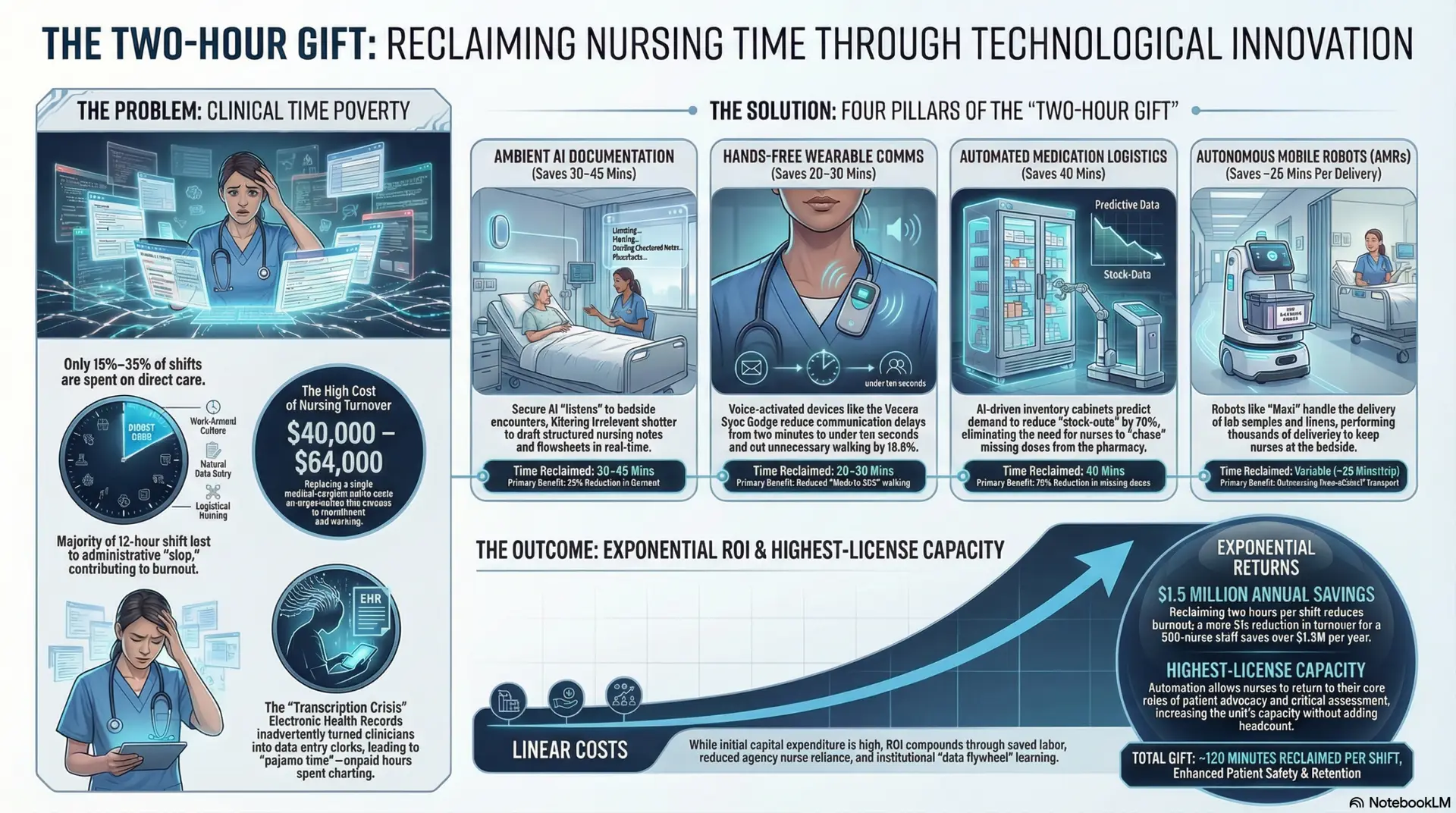
I’ve seen firsthand how the demands on nurses time have intensified. We are facing a critical moment in healthcare. Burnout rates among clinicians are at unsustainable levels, exacerbated by persistent staffing shortages. Perhaps the most frustrating contributor to this crisis is the “administrative time-sink.” Studies have shown that nurses can spend up to a staggering 40% of their shift on documentation and data entry, taking precious time away from direct patient care (Vehko et al., 2019).
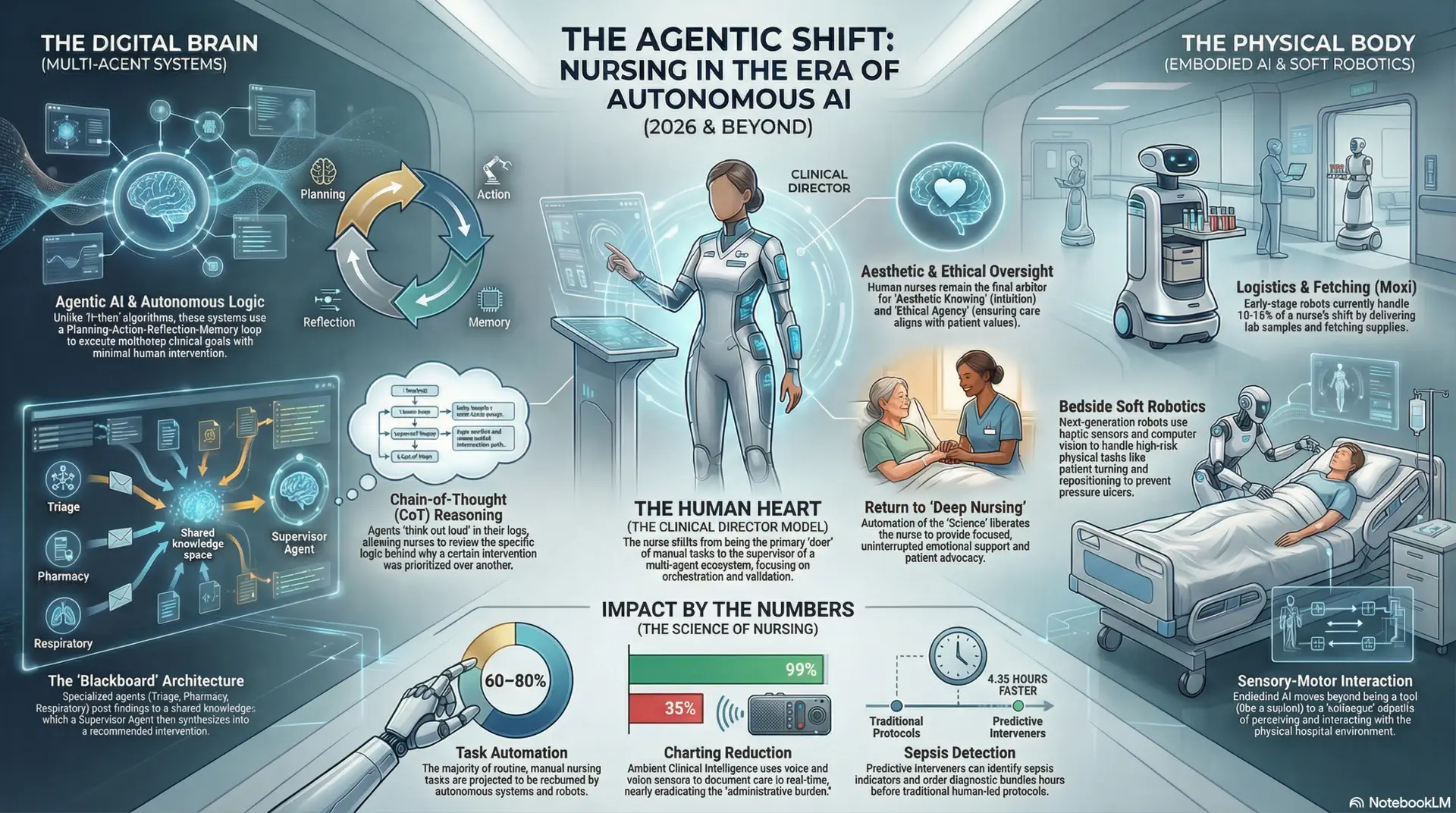
We need a change. We need tools that don’t just add another layer of technology but actually alleviate the burden. This brings us to the concept of the “AI-Enhanced Nursing Environment.” We are looking ahead to a near future—2026 and beyond—where Artificial Intelligence (AI), specifically advanced AI chatbots (built on Large Language Models), will become integral members of the care team.
Think of these not as search engines, but as “virtual colleagues” or “cognitive partners.” The thesis of this discussion is simple yet transformative: AI chatbots represent a paradigm shift in nursing, moving us from a model of manual data entry to one of “data curation.” This shift is the key to unlocking your time and allowing you to return to what you do best: “top-of-license” bedside care.
II. Theoretical Framework: The Shift in Workflow
To understand this future, we must first look at how our work is organized today.
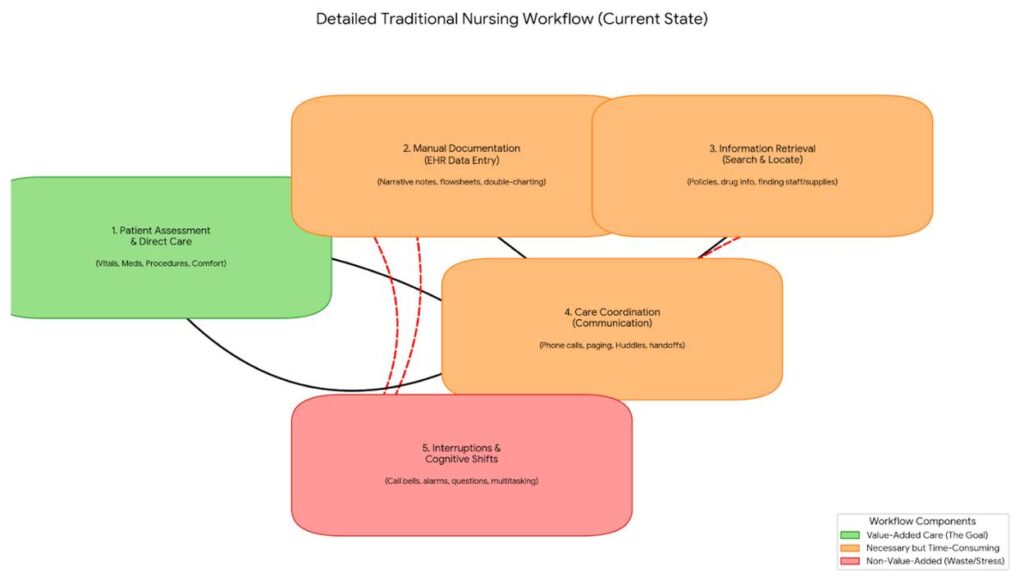
From Interruption to Integration
Our current systems are often sources of interruption. A call bell rings, a phone buzzes, an alert pops up on a screen—each one breaks your focus and pulls you away from the patient in front of you. AI-mediated communication aims to change this by moving from a disruptive model to an integrated one. Instead of a raw signal (a bell), an AI system can triage and contextualize information. For example, an AI could differentiate between a patient asking for water and one reporting chest pain, routing the request to the appropriate personnel (e.g., a PCA vs. an RN) without an intrusive alert for every single event.
Cognitive Load Theory
Nursing is cognitively demanding. Every shift requires you to hold vast amounts of patient data in your head, constantly prioritize tasks, and make split-second decisions. This mental effort is called cognitive load. When you have to stop what you’re doing to log into a computer, navigate a complex intranet to find a hospital policy, or look up a drug interaction in a separate database, you are adding extraneous cognitive load—mental work that doesn’t directly contribute to patient care (Sweller, 2011).
AI chatbots are powerful tools for reducing this extraneous load. Instead of a multi-step search process, you could simply ask an AI assistant, “What is the protocol for a heparin drip infusion?” or “Does this patient’s new antibiotic interact with their current heart medication?” The AI performs the information retrieval and synthesis instantly, presenting you with the answer so you can apply it. This frees up your mental energy for critical thinking and clinical judgment.
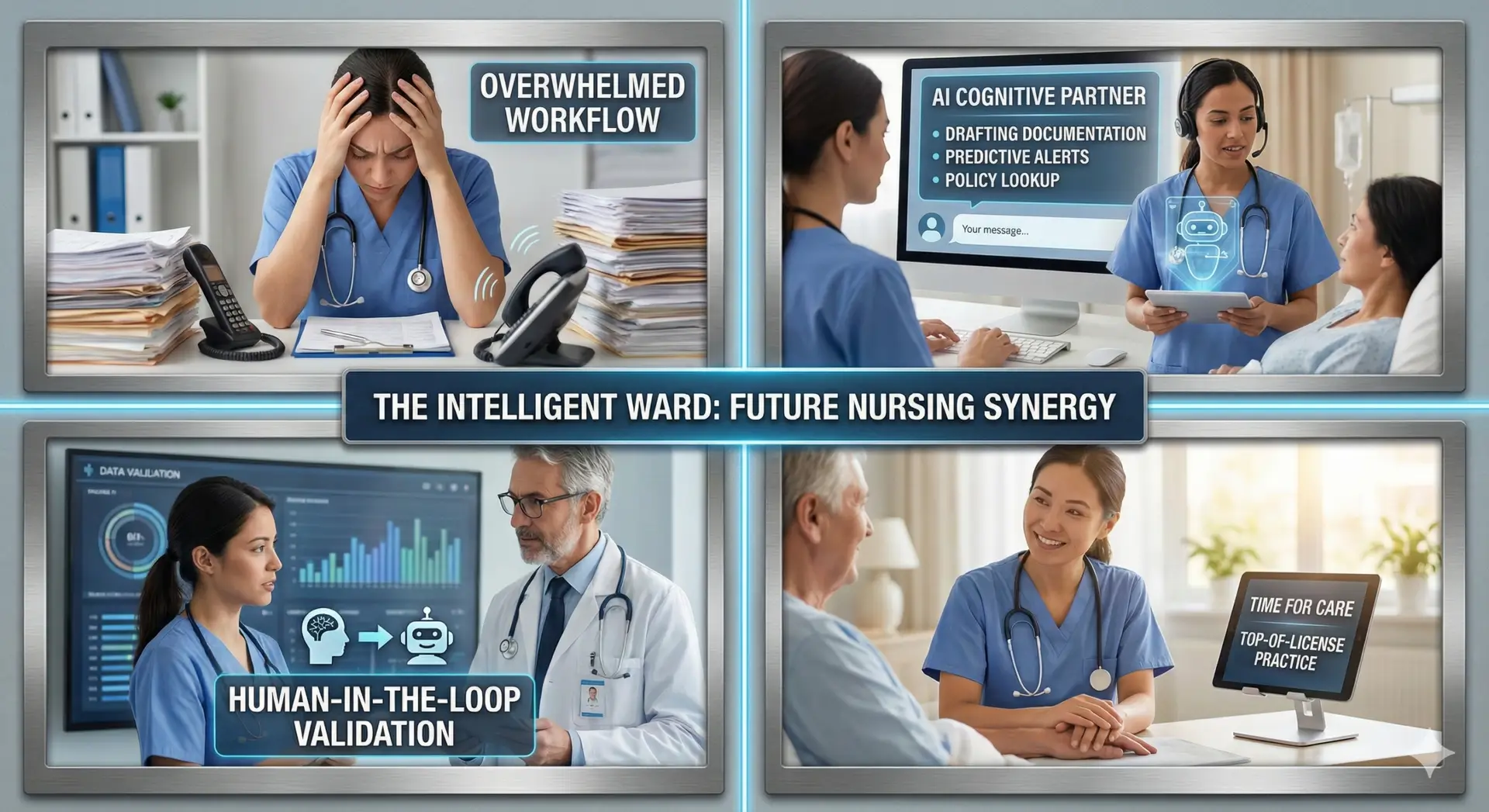
The “Human-in-the-Loop” Model
A common fear is that AI will replace nurses. This is a misconception. The scholarly and practical consensus supports a “Human-in-the-Loop” model. In this framework, AI systems are designed to augment, not replace, human expertise.
As illustrated, the AI acts as a sophisticated assistant. It processes vast amounts of data from the Electronic Health Record (EHR), vitals monitors, and other sources. It then analyzes this data to draft documentation or suggest a course of action. However, the process does not end there. The crucial final step is Nurse Validation. You, the human expert, must review the AI’s output, apply your clinical judgment and contextual knowledge of the patient, and then make the final decision. You remain in control, and your license is the ultimate authority.
Figure 1. The ‘Human-in-the-Loop’ Model for Clinical AI
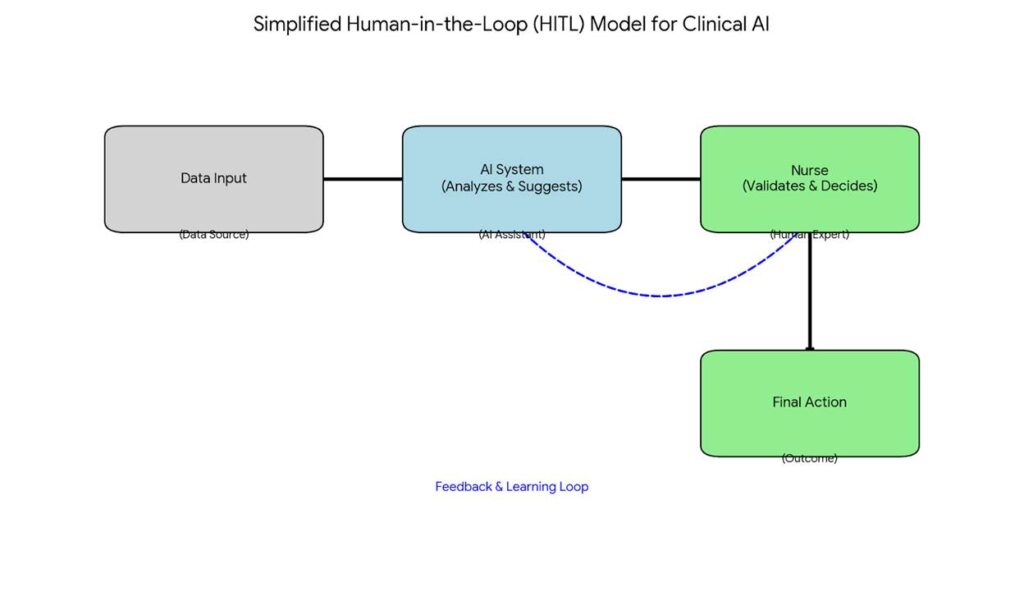
Note. This diagram illustrates the flow of information where the AI acts as a preparatory tool, and the nurse provides the final, critical validation.
III. Strategic Applications for Nursing Workflow
Let’s look at concrete ways this technology will change your daily routine. Figure 2 provides a high-level comparison of a traditional versus an AI-enhanced workflow.
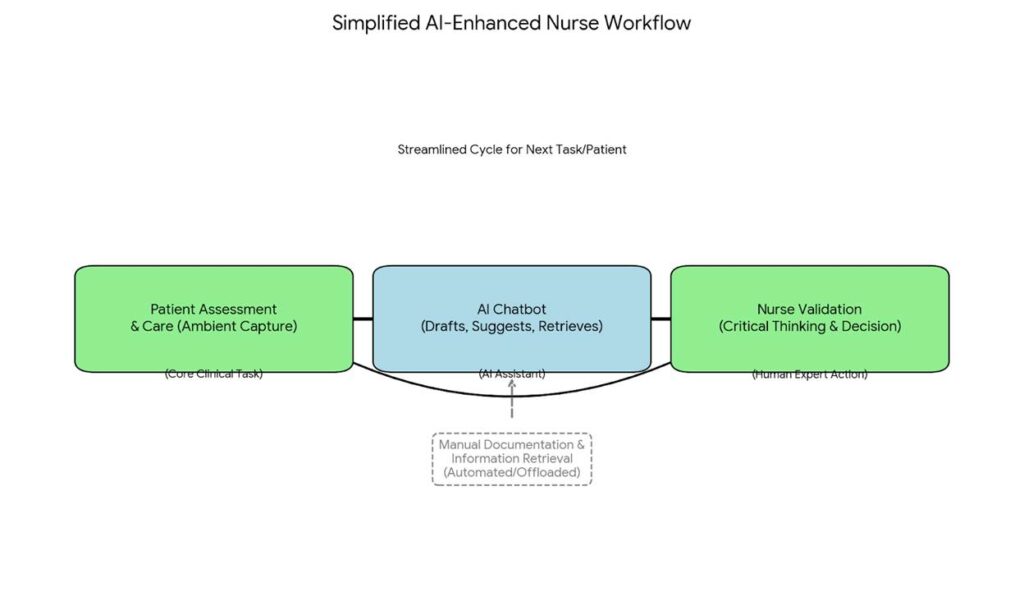
Ambient Clinical Documentation
Imagine a future where you no longer have to spend hours at the end of your shift “catching up on charting.” Ambient clinical documentation uses AI to listen (with patient consent) to your interaction with a patient at the bedside. The AI then automatically synthesizes that conversation into a structured note within the EHR.
- Example: As you perform a wound dressing change, you narrate your observations to the patient: “The wound bed is clean, with good granulation tissue. The measurements are 3cm by 2cm. I’m applying a new foam dressing.” The ambient AI captures this and drafts a perfect procedure note. You simply review and sign it. This shifts your role from a data entry clerk to a data curator and validator.
Figure 2. Traditional vs. AI-Enhanced Nursing Workflow Comparison
Note. This comparison highlights how AI integration removes repetitive manual tasks and interruptions, creating a more direct path from assessment to validated care.
Predictive Decision Support (PDS)
Current alarm systems are reactive; they alert you when a patient’s vitals have already crossed a dangerous threshold. AI-powered Predictive Decision Support is proactive. By analyzing trends across hundreds of data points in real-time, an AI chatbot can identify subtle patterns that may indicate deterioration hours before a traditional alarm would trigger.
- Example: An AI agent might send you a secure message: “Nurse Sarah, Patient Jones in Room 312 is showing a 15% trend upward in heart rate and a slight drop in blood pressure over the last 4 hours, combined with their recent lab results. This pattern is consistent with early sepsis. Would you like to review the sepsis protocol?” This “nudge” allows you to intervene earlier, potentially preventing a crisis.
Dynamic Resource & Shift Management
The administrative burden isn’t just about patient charts; it’s also about managing the unit. AI agents can handle these logistical tasks.
- Example: Instead of calling central supply or hunting for equipment, you could simply say to a unit’s smart speaker, “AI, we are out of 20-gauge IV start kits in the clean utility room.” The AI agent instantly places an order with the supply chain system. Similarly, AI can help with real-time staffing by predicting unit acuity and suggesting adjustments to the charge nurse, moving from reactive to dynamic resource management.
IV. Enhancing Support Systems for Professional Growth
AI is not just about workflow efficiency; it’s a powerful tool for your professional development.
Real-time Clinical Mentorship
No nurse can know everything, especially with the rapid pace of medical advancement. An AI chatbot can act as an always-available mentor.
- Example: You are assigned a patient with a rare condition requiring a procedure you haven’t performed in two years. Instead of feeling unsure or frantically searching through manuals, you can ask the unit’s “Policy Bot”: “Walk me through the steps for a bedside thoracentesis setup according to our hospital’s latest policy.” The bot provides a step-by-step guide, instantly refreshing your knowledge and ensuring adherence to evidence-based practice.
Onboarding and Continuous Education
For new graduates or nurses transferring to a new specialty, the learning curve is steep. AI can deliver personalized “micro-learning” modules directly within the workflow.
- Example: During orientation, a new nurse could interact with a chatbot to practice charting scenarios in a safe, simulated environment. The AI provides immediate feedback, helping build confidence and competence faster than traditional methods.
V. Critical Ethical and Scholarly Considerations
As excited as we are about this future, we must approach it with critical thinking and ethical vigilance.
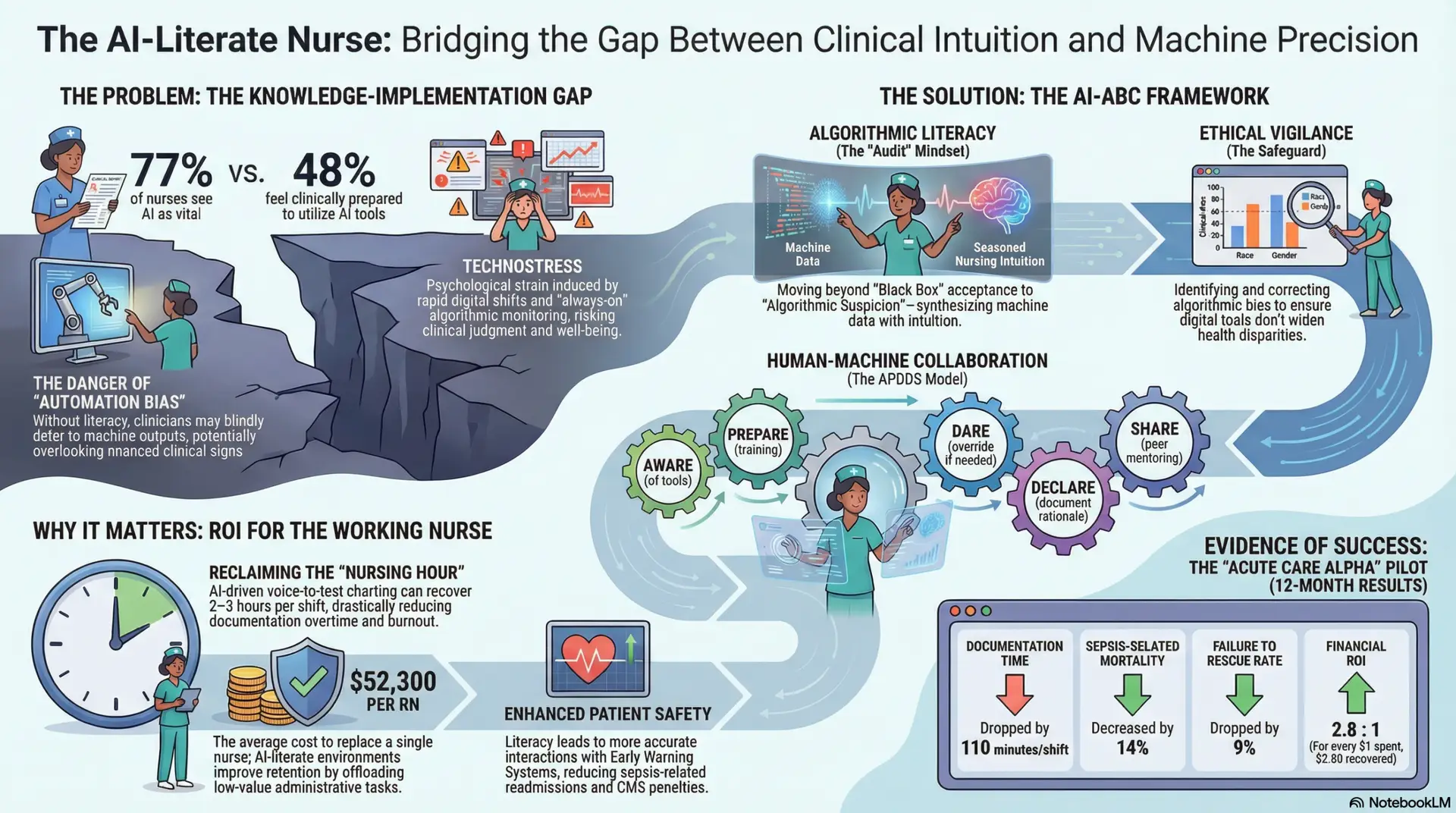
Algorithmic Bias and Equity
AI models are trained on vast datasets of historical data. If that data contains historical biases in how care was delivered to different patient populations (e.g., based on race, gender, or socioeconomic status), the AI can learn and perpetuate those biases (Obermeyer et al., 2019). We must demand transparency from AI developers and continuously audit these systems to ensure they promote health equity, not disparity.
Data Privacy (HIPAA 2.0)
Protecting patient privacy is paramount. The integration of generative AI introduces new challenges. We need robust frameworks—a “HIPAA 2.0″—that ensure patient data used to prompt AI chatbots is de-identified and secure, and that the data is not used to train public models outside the healthcare system’s control.
The Preservation of Nursing Intuition
Finally, we must guard against “automation complacency.” There is a risk that nurses could become over-reliant on AI suggestions, accepting them without question. This could erode critical thinking skills and the “art of nursing”—that intuitive sense that something is wrong with a patient even when the numbers look fine. The “Human-in-the-Loop” model is our primary defense against this. Nursing education must emphasize that AI is a tool to inform your judgment, never to replace it.
VI. Conclusion: The Future Horizon
In conclusion, the integration of AI chatbots into nursing is not about replacing you. It is about creating a force multiplier for your expertise. By offloading the cognitive burden of information retrieval and the repetitive tasks of documentation, AI can free you to practice at the top of your license.
The future of nursing is not human or AI; it is human plus AI. To realize this potential, we must be active participants in this transformation. We need nursing leaders and educators to champion AI literacy, ensuring that every nurse has the knowledge and skills to use these powerful tools ethically and effectively. The most effective nurse of the future will be the one who expertly combines their human compassion and clinical judgment with the capabilities of intelligent technology.
References
- Obermeyer, Z., Powers, B., Vogeli, C., & Mullainathan, S. (2019). Dissecting racial bias in an algorithm used to manage the health of populations. Science, 366(6464), 447-453. https://doi.org/10.1126/science.aax2342
- Sweller, J. (2011). Cognitive load theory. In J. P. Mestre & B. H. Ross (Eds.), The psychology of learning and motivation: Cognition in education (Vol. 55, pp. 37–76). Elsevier Academic Press. https://doi.org/10.1016/B978-0-12-387691-1.00002-8
Vehko, T., Hyppönen, H., Piri, H., Ryhänen, M., & Heponiemi, T. (2019). Hospital nurses’ working conditions, strengths and work-related needs in the era of digitalized work environments. Finnish Journal of EHealth and EWelfare, 11(4), 273–283. https://doi.org/10.23996/fjhw.83456