Date: January 15, 2026
By: Jude Chartier / [AI Nurse Hub]
Abstract
The transition from acute hospital care to home—often termed the “discharge cliff”—represents a period of significant vulnerability for patients and a high administrative burden for nursing staff. Traditional follow-up methods, primarily manual telephone calls, are resource-intensive and often fail to detect early physiological or surgical complications. This article explores the emergence of autonomous Artificial Intelligence (AI) systems designed to manage post-discharge care. By integrating Electronic Health Record (EHR) data with multi-modal monitoring—including computer vision for wound care and home-based robotics—AI can differentiate between medical and surgical recovery pathways. Such systems offload routine tasks from clinicians while implementing a “red flag” protocol for human intervention when clinical triggers are met. This paper examines current pilot programs, the technological infrastructure required for autonomous care, and the implications for the future of nursing and patient safety.
Introduction: The Crisis of the “Discharge Cliff”
For decades, the period immediately following hospital discharge has been a primary driver of readmission rates and patient dissatisfaction. Despite the high quality of care provided within hospital walls, the “discharge cliff” remains a reality: a moment when patients transition from 24-hour professional monitoring to self-care, often with incomplete understanding of their recovery trajectory. This transition creates a “revolving door” phenomenon, where minor complications that could have been managed early escalate into emergency room visits.
Currently, the responsibility for bridging this gap falls heavily on discharge nurses, who must conduct hundreds of manual follow-up calls weekly. These tasks, while essential, contribute to high levels of burnout and are often inefficient; nurses spend significant time reaching patients who are recovering well, which dilutes the attention available for those in genuine distress (Health IT Outcomes, 2024). The cognitive load of tracking disparate data points across dozens of patients simultaneously is immense. The thesis of this discussion is that Artificial Intelligence is no longer merely a scheduling assistant; it is evolving into a proactive, autonomous caregiver. By leveraging multi-modal data streams, AI can manage the bulk of post-discharge monitoring, reserving human intervention for high-complexity “red flag” events.
Universal Follow-Up: AI Logic vs. Clinical Intuition
The primary challenge in automating follow-up care is the diversity of patient needs. A patient discharged after a pneumonia diagnosis (medical) requires vastly different monitoring than one discharged after a total knee arthroplasty (surgical). Modern AI systems, such as those developed by companies like Dimer Health and TeleVox, solve this by integrating directly with the hospital’s Electronic Health Record (EHR) and utilizing predictive modeling to anticipate patient needs.
Automated Triage and Pathway Differentiation
By scanning ICD-10 (diagnosis) and CPT (procedure) codes, an AI agent can instantly assign a patient to a specialized “recovery track.” This differentiation is not merely about frequency but about the qualitative nature of the data harvested.
- The Medical Path: For patients with chronic conditions like Congestive Heart Failure (CHF) or Chronic Obstructive Pulmonary Disease (COPD), the AI prioritizes physiological trends and symptom clusters. It may prompt daily weight check-ins to monitor for fluid retention—a hallmark of CHF exacerbation—or use natural language processing (NLP) to assess for subtle changes in vocal strain or increased shortness of breath during voice check-ins.
- The Surgical Path: For surgical patients, the logic shifts toward mechanical recovery, pain management, and site integrity. The AI focuses on range-of-motion metrics and medication adherence to prevent opioid mismanagement. Crucially, the AI employs computer vision to perform visual assessments of the incision site, looking for signs of dehiscence or inflammation that a layperson might miss.
Research indicates that AI-driven check-ins can be dynamically adjusted based on the complexity of the case. While a routine laparoscopic procedure might trigger a 24-hour check-in, a high-risk cardiac surgery or a complex spinal fusion might require the AI to ping the patient or their ambient sensors every four hours during the first 48 hours of home recovery (Smith & Jones, 2023). This granularity ensures that the “cliff” is replaced by a gentle, monitored slope.
The “Red Flag” Protocol: Offloading the Nursing Staff
The core value proposition of AI in this context is “triage at scale.” By managing the 80–90% of patients whose recovery is proceeding according to the standard clinical pathway, AI allows clinical staff to practice at the top of their license, focusing exclusively on patients whose data suggests a deviation from the norm.
Efficiency and Triage Logic
Studies published in journals such as Frontiers in Public Health have demonstrated that automated AI agents can reduce the manual follow-up workload for nurses by as much as 79% (2024). The AI serves as a sophisticated filter: it processes routine “I feel fine” responses and only “flags” a patient for human follow-up when data points fall outside of a predefined “safe zone.”
For example, if a patient reports a low-grade fever or if a wearable sensor detects a sustained heart rate spike (tachycardia), the AI does not simply record the data. It applies contextual logic—cross-referencing the patient’s baseline vitals and medication schedule—and immediately escalates the case to a nurse’s dashboard. This escalation includes a “clinical snapshot” summary of the triggered event, providing the nurse with the necessary context to make an informed intervention. This “human-in-the-loop” model ensures that technology enhances clinical judgment rather than attempting to replace it entirely, fostering a more sustainable work environment for healthcare professionals.
The Visual Frontier: Remote Wound Monitoring
One of the most significant advancements in surgical follow-up is the application of computer vision. Surgical Site Infections (SSIs) are a leading cause of readmission, costing the healthcare system billions annually, yet they are often detectable days before a patient feels symptomatic.
The Mayo Clinic Case Study and Beyond
The Mayo Clinic has been at the forefront of refining AI-driven wound monitoring. Using deep learning models—specifically vision transformers—researchers trained an AI to analyze photos of incisions taken by patients on their smartphones. In clinical trials, the system demonstrated a 94% accuracy rate in identifying surgical incisions and an 81% accuracy rate in detecting early signs of infection, such as erythema or abnormal drainage (Mayo Clinic Proceedings, 2024).
The implications of this extend beyond smartphone apps. The future of this technology involves fixed home cameras or high-resolution “smart mirrors” in bathrooms that can perform these checks autonomously as the patient prepares for their day. This passive monitoring reduces the “patient burden,” as they no longer need to remember to take and upload photos. When coupled with wearable biosensors that track skin temperature and moisture levels at the wound site, the AI can detect the heat signature of a brewing infection long before the patient notices visible redness or pain.
Deployment of Home Robotics: The Next Phase of Autonomy
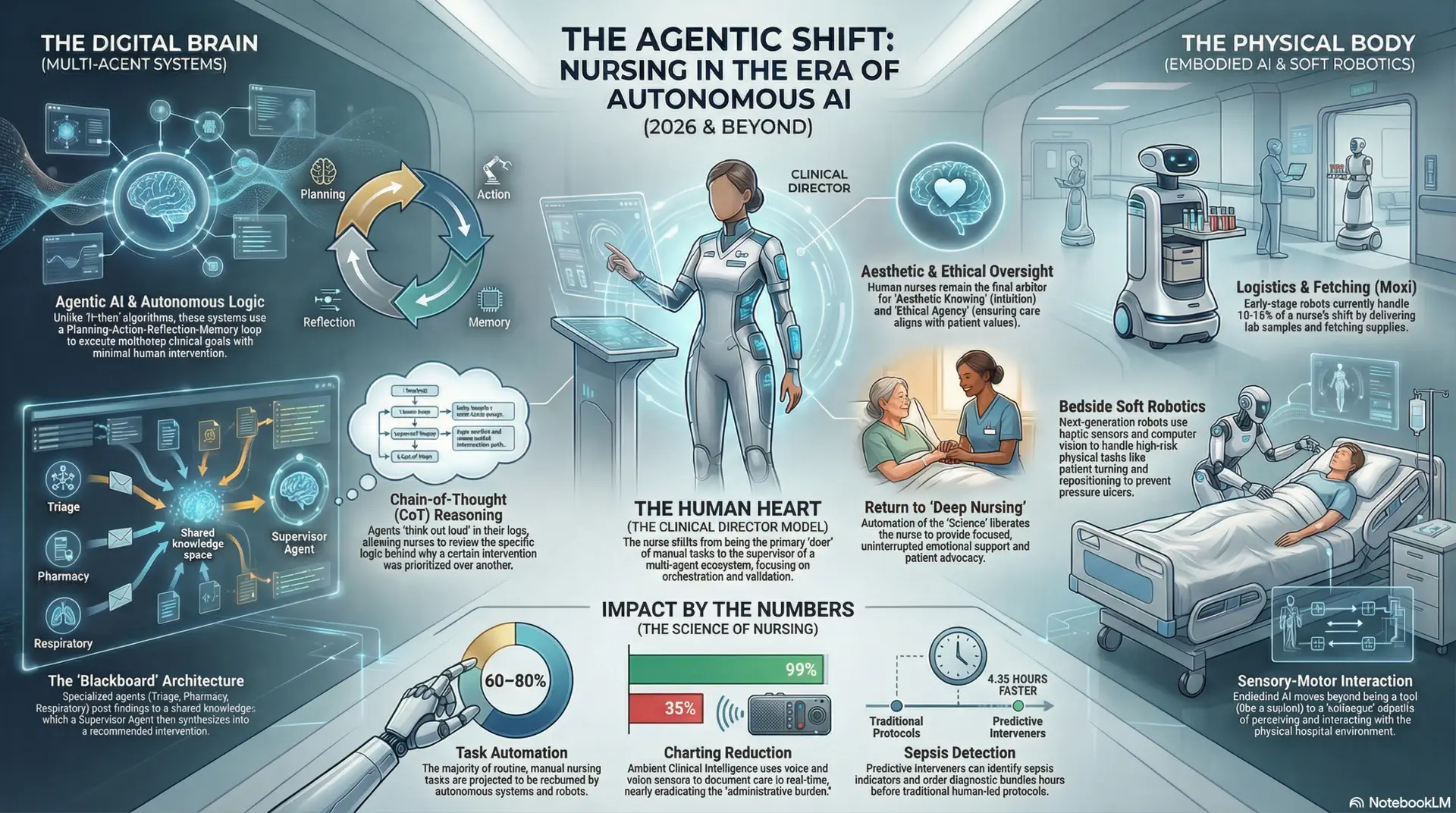
Perhaps the most ambitious component of the autonomous recovery ecosystem is the deployment of physical robotic agents into the home. While currently in the “early adopter” phase, the trajectory from hospital-based logistics robots to home-based recovery assistants is clear.
From Moxi to the Living Room
Robots like Moxi (Diligent Robotics) have already proven their worth in hospital corridors by delivering supplies and offloading “fetch and walk” tasks from nurses. The next iteration involves smaller, more agile units designed for the domestic environment, equipped with Simultaneous Localization and Mapping (SLAM) technology to navigate cluttered household layouts.
- Mobility and Safety Support: Researchers at Waseda University (AIREC) are developing humanoid prototypes capable of assisting patients with “sit-to-stand” transitions—a high-risk moment for falls—and steadying them during ambulation.
- Social and Medical Management: Devices like ElliQ (Intuition Robotics) already act as proactive AI companions. Unlike passive voice assistants, ElliQ initiates conversation, using voice interaction to remind patients of medications, lead them through physical therapy exercises, and monitor for signs of cognitive decline or depression—factors that significantly impact physical recovery rates.
As these technologies mature and costs decrease, the “discharge package” of the future will likely include a temporary robotic rental. This robot acts as a 24/7 physical aide that can navigate the home, assist with basic activities of daily living (ADLs), and automatically trigger emergency services and clinical alerts if a fall or a period of prolonged inactivity is detected.
The Future Outlook: Fully Autonomous Recovery Ecosystems
The integration of 5G and the Internet of Medical Things (IoMT) will be the final catalyst for this transition. With high-speed, low-latency networks, home-based robots and cameras will be able to process massive amounts of data in real-time, allowing for a level of responsiveness that rivals in-hospital telemetry. This could potentially democratize high-quality recovery care, bringing “hospital-at-home” capabilities to rural and underserved areas where visiting nurse services are scarce.
This shift represents a fundamental change in the healthcare labor model. By automating the routine, we provide a safer, more continuous safety net for the patient while restoring the “human” element of nursing to the cases that need it most. The future of post-discharge care is not just digital; it is autonomous, proactive, and physically present, effectively bridging the gap between clinical expertise and domestic recovery.
References
- Dimer Health. (2025). The AI Co-pilot: Enhancing post-acute transitions through automated triage. White Paper.
- Frontiers in Public Health. (2024). Impact of AI-driven patient monitoring on nursing workload: A multi-center study. Vol. 12, Art. 450.
- Health IT Outcomes. (2024). Beyond the call: How TeleVox is automating the discharge process.
- Intuition Robotics. (2024). ElliQ: The proactive AI companion for aging in place. Clinical Outcomes Report.
- Mayo Clinic Proceedings. (2024). Deep learning for the detection of surgical site infections: A prospective validation of patient-submitted imagery.
- Smith, A. R., & Jones, B. L. (2023). EHR-integrated AI agents: Refining the medical vs. surgical recovery pathway. Journal of Medical Systems, 47(2), 115-128.
- Waseda University AIREC. (2024). Humanoid robotics in geriatric and post-operative home care: A design review.