Date: January 7, 2026
By: Jude Chartier [AI Nurse Hub]
Introduction: The New Clinical Reality
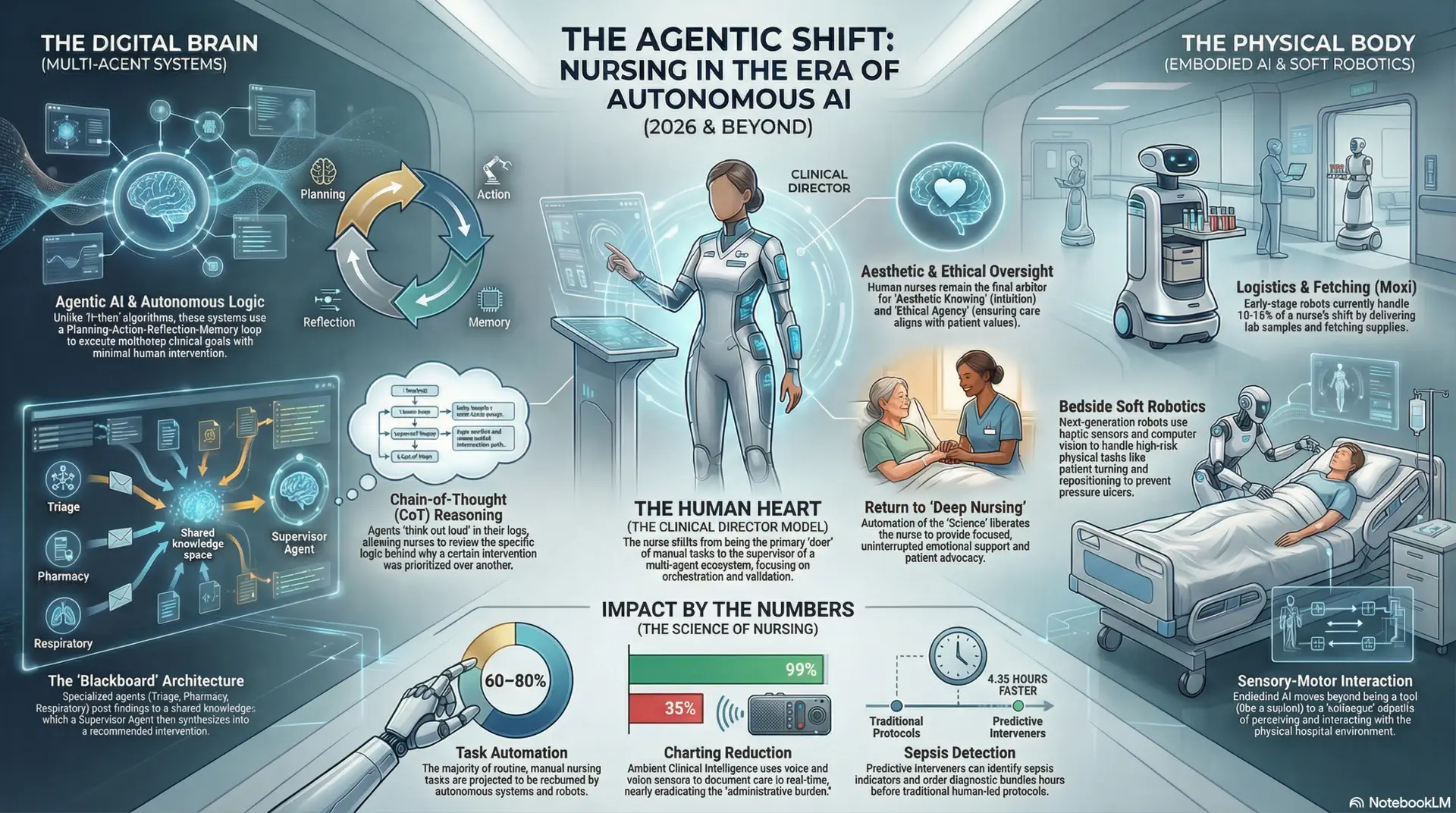
In the near future, nursing will no longer be defined solely by physical presence at the bedside. The modern healthcare environment, characterized by virtual wards, highly complex patient acuities, and a deluge of real-time data from the Internet of Medical Things (IoMT), has necessitated a fundamental shift in clinical practice. We have moved from an era of reactive care—responding to deterioration after it becomes symptomatic—to an era of proactive, predictive medicine.
At the center of this shift is Artificial Intelligence (AI) predictive analysis. This technology is not a futuristic concept; it is the operational backbone of modern health systems. The urgent question facing the nursing profession today is no longer “Will AI affect my job?” but rather, “Do I possess the necessary skills to partner effectively with these powerful algorithmic tools?”
This article examines the critical role of nurses in the age of predictive intelligence, outlines the essential new skills required for competency, and argues that fluency in AI is no longer optional—it is the deciding factor between a struggling nurse and a highly effective, future-ready clinician.
De-Mystifying Predictive Analysis in Healthcare
To master a tool, one must first understand its function. In healthcare, predictive analytics utilizes historical data, statistical algorithms, and machine learning techniques to determine the likelihood of future outcomes based on what has happened in the past (National Institutes of Health [NIH], 2024).
Unlike traditional monitoring, which tells a nurse what a patient’s vital signs are right now, predictive AI analyzes the trajectory. It continuously scans vast datasets—including lab results, vital sign trends from wearable sensors, unstructured nursing notes via Natural Language Processing (NLP), and even social determinants of health—to identify subtle patterns invisible to the human eye.
These systems currently monitor and alert for critical events such as:
- Sepsis onset hours before clinical symptoms manifest.
- Likelihood of hospital readmission within 30 days.
- Acute kidney injury (AKI) risk based on medication administration and hydration status.
- General clinical deterioration (often summarized by composite scores like the Rothman Index), flagging patients who are “crashing silently” (Frontiers in Medicine, 2025).
Crucially, predictive analysis does not exist in a vacuum. In advanced settings like 2026 virtual hospitals, predictive algorithms act as the “central nervous system,” interacting with other AI technologies. For example, if a predictive model calculates a high fall risk for a home-based patient, it may automatically trigger an embodied humanoid robot in the home to move closer to the patient for standby assistance, while simultaneously alerting the virtual nurse to initiate a safety consultation (Zachariae et al., 2024).
The Nurse’s Role: The Indispensable “Human-in-the-Loop”
There is a pervasive myth that AI automation removes the need for human judgment. The opposite is true. The more sophisticated the AI, the more critical the human nurse becomes as the “human-in-the-loop.”
AI models provide a mathematical probability, not an absolute clinical certainty. The nurse’s role shifts from primarily data collection to high-level data synthesis and contextualization. A predictive model might flag a patient for deterioration based on rising heart rate and dropping blood pressure. However, it is the nurse who knows the patient just finished a taxing physical therapy session and is experiencing expected, transient physiological changes.
The nurse serves as the ethical and clinical firewall between the algorithm’s raw output and the patient’s actual care plan. Without this human contextualization, predictive analytics can lead to “alarm fatigue,” unnecessary interventions, and depersonalized care (Wieben et al., 2025).
The New Essential Skills: A Call to Upskill
To effectively fulfill this role, the nursing competency framework must expand. Proficiency in starting IVs and auscultating lung sounds remains vital, but it is no longer sufficient. Nurses who wish to remain competitive and competent must develop the following skills:
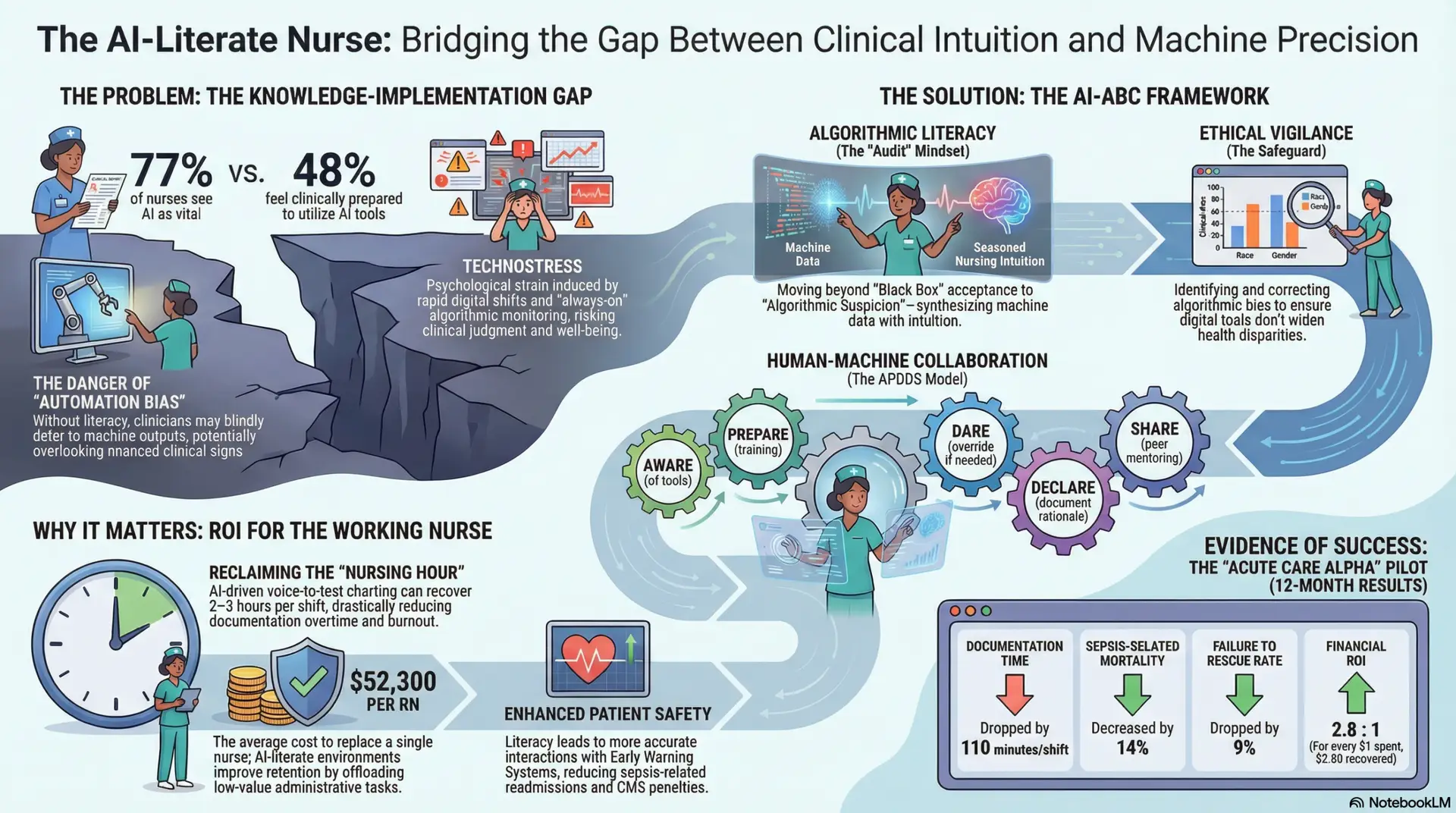
1. Algorithmic Literacy and “Data Detective” Work
Nurses do not need to learn python coding, but they must understand the basic “logic” of the models they use. This means asking critical questions: What data is this prediction based on? When was the model last updated? Is the data representative of my specific patient population? A nurse must be able to investigate why an alert fired, rather than blindly accepting it.
2. Combating Automation Bias through Critical Thinking
A significant risk in high-tech environments is “automation bias”—the tendency for humans to favor suggestions from automated decision-making systems and to ignore contradictory information made without automation, even when they are correct (Frontiers in Digital Health, 2025).
Nurses must be trained to maintain a healthy skepticism of AI outputs. The skill lies in recognizing when clinical intuition contradicts the algorithm and having the confidence and institutional support to override the machine. This requires advanced pathophysiology knowledge to articulate why the AI might be wrong in a specific instance.
3. Interoperable Systems Management
Nurses must understand how predictive data flows through the healthcare ecosystem. A predictive alert regarding medication non-adherence in a virtual patient, for instance, might require the nurse to coordinate not just with the physician, but also with the patient’s in-home robotic assistant to verify pill counts, and the pharmacy AI to adjust delivery schedules. Managing these intersecting digital workflows is now a core nursing responsibility.
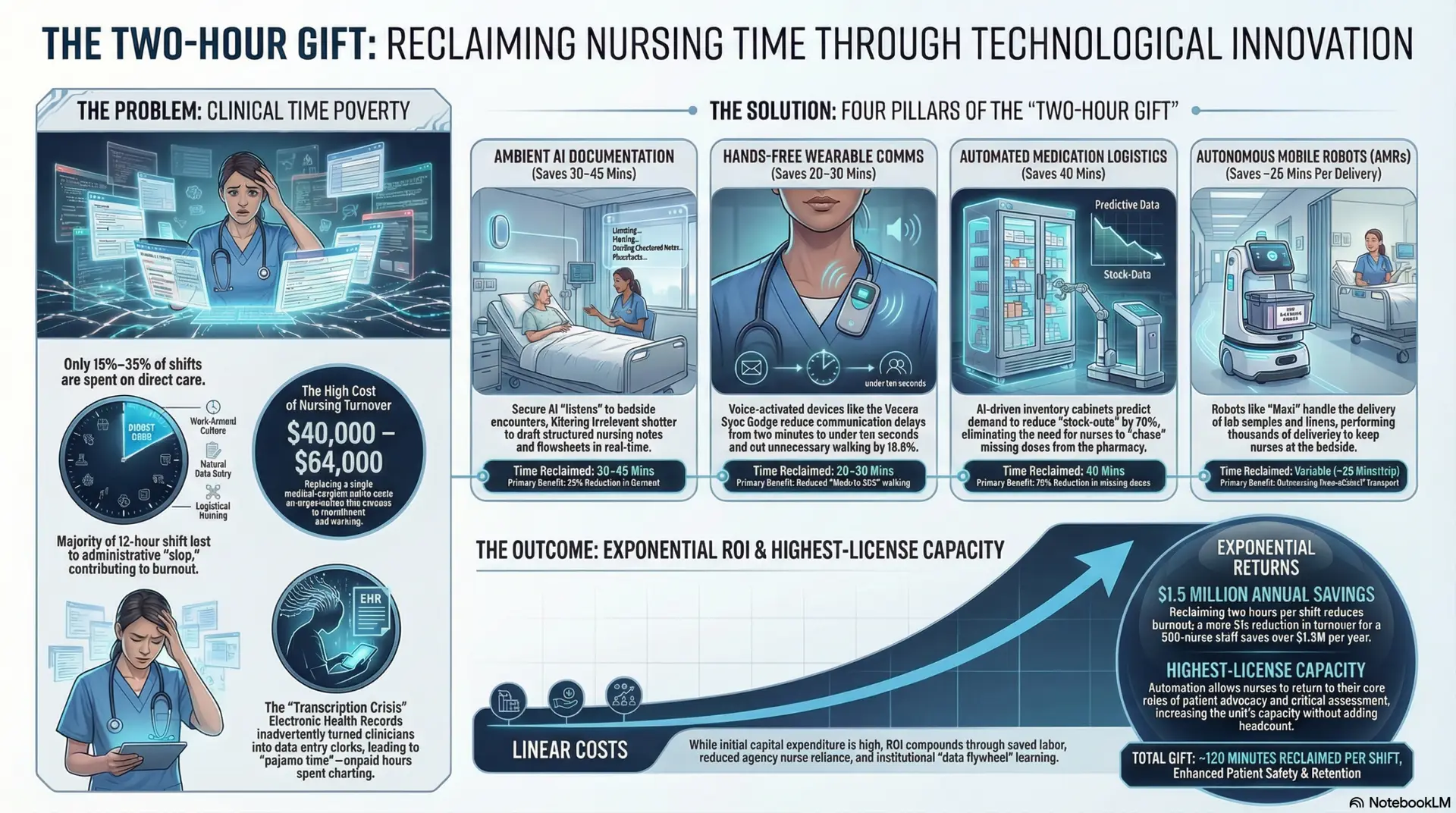
The Imperative: Adapt or Be Left Behind
The integration of predictive AI is creating a bifurcation in the nursing workforce. On one side are nurses who embrace these tools as powerful augmentations to their practice. These nurses experience reduced administrative burden, can manage higher acuity patient loads safely, and often identify life-threatening complications earlier (American Hospital Association [AHA], 2025).
On the other side are nurses who resist or ignore these technologies due to lack of training or fear. These nurses are at a distinct disadvantage. They are working harder, relying solely on manual assessments in an environment designed for digital speed, and potentially missing critical early warning signals that their AI-enabled colleagues catch readily.
Furthermore, healthcare systems hiring in 2026 are increasingly viewing digital fluency not as a “nice-to-have” bonus, but as a baseline competency equivalent to basic life support (BLS) certification.
Conclusion
The arrival of AI predictive analysis does not signal the end of compassionate, human-centered nursing. Rather, it signals the end of nursing based on reactive guesswork and incomplete data. By mastering the skills of algorithmic literacy, critical thinking against automation bias, and digital systems management, nurses can ensure they remain the master of these new tools, using them to elevate the profession and improve patient outcomes in ways previously unimaginable. The future belongs to the AI-augmented nurse; the time to prepare is now.
References
American Hospital Association. (2025). Innovation and the future of the nursing workforce: Redefining care delivery in the digital age. https://www.aha.org/center/emerging-issues/workforce
Frontiers in Digital Health. (2025). Trust me, I’m a robot: Automation bias in healthcare and strategies for mitigation. https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1478921/full
Frontiers in Medicine. (2025). The integration of AI in nursing: Addressing current applications, challenges, and future directions. https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1545420/full
National Institutes of Health. (2024). Predictive analytics in healthcare: Opportunities and challenges. PMC11221308. https://pmc.ncbi.nlm.nih.gov/articles/PMC11221308/
Wieben, A., et al. (2025). Advancing nursing practice through artificial intelligence: Unlocking its transformative impact. Online Journal of Issues in Nursing (OJIN). https://ojin.nursingworld.org/
Zachariae, M., et al. (2024). Examining the role of AI in changing the role of nurses in patient care: A systematic review. PubMed Central. https://pmc.ncbi.nlm.nih.gov/articles/PMC11888071/